Background
Bronchiolitis obliterans syndrome (BOS) is a life-threatening pulmonary manifestation of chronic graft versus host disease (cGVHD) post-allogeneic hematopoietic stem cell transplantation (HSCT), without a clear standard of care. Systemic corticosteroids remain the backbone of therapy for BOS, but their side effect profile makes them disadvantageous for prolonged use. Ruxolitinib (RUXO), a Janus-associated kinase (JAK) 1/2 inhibitor approved for the treatment of patients with intermediate-2 or high-risk primary myelofibrosis,has shown excellent response rates in steroid-refractory/intolerant cGVHD. This study seeks to investigate the efficacy of ruxolitinib on steroid-refractory BOS, and additionally, determine the efficacy of ruxolitinib in these patients and the clinical factors affecting the response to ruxolitinib.
Method
This study involved adult patients suffering BOS after an allogeneic HSCT for a hematological malignancy between January 2014 and June 2018 at the First Affiliated Hospital of Zhejiang University School of Medicine and Ningbo Hospital of Zhejiang. Univariable analyses for treatment response risk factors were performed using the Fisher exact test and chi-square test. Logistic regression analysis was used to perform multivariable analysis to calculate the hazard ratio (HR) with a 95% confidence interval (CI). Overall survival (OS) was defined as the time from stem cell infusion to death from any cause and calculated by the Kaplan-Meier method.
Results
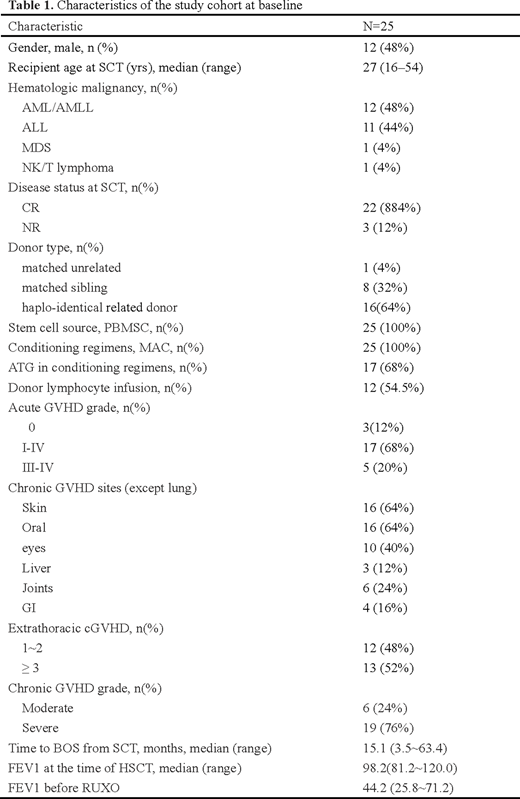
Twenty-five patients were retrospectively enrolled in this analysis and patient characteristics were shown in Table 1. At the time of BOS diagnosis, most patients presented with moderate or severe obstruction. Besides, all patients had worsening lung function or worsening clinical symptoms under systemic prednisone treatment. After a median duration of RUXO therapy of 8.5 (1.5-20) months, the overall response rate was 68.0%: two patients (8.0%) achieved complete remission, and 15 (60.0%) achieved partial remission. The median time from initiation of RUXO to achieve the best responses was 3 months (range, 1.5-8). Since initiating RUXO, predicted forced expiratory volume in 1 s (FEV1) % increased after 3 months and 6 months compared with measurements before RUXO in responders. Of note, an average reduction in prednisone dose of 39.3% after 3 months of ruxolitinib therapy and 59.5% after 6 months of ruxolitinib therapy was reported. Only FEV1 mild decline before ruxolitinib with a ratio ≤15% was an independent predictor to achieve a response to RUXO (HR = 0.063, 95% CI 0.006-0.624, P = 0.018). As for safety profile, hematological adverse effect included that two patients harboring cytopenia with grade 2-3. Regarding the nonhematological toxicities, two patients developed grade 3 hypertriglyceridemia. Referring to infection events, 11 patients (44%) had a severe pulmonary infection of ≥3 grade. Of note, cytomegalovirus (CMV) DNAemia was observed in 3 patients (12%) and Epstein-Barr virus (EBV) DNAemia was observed in 10 patients (40%). Following a median follow-up of 255 days after RUXO, the 2-year incidence of nonrelapse mortality and 2-year overall survival rate after RUXO among patients with BOS was 27.8% and 62.6%, respectively.
Conclusion
The present study showed that in heavily pretreated patients with BOS, ruxolitinib induced a relatively high response, leading to an increased 2-year OS rate in patients with BOS. Although a small number of subjects and a retrospective nonrandomized design of this study might make a bias, our data still indicated RUXO as a promising treatment option to improve the prognosis of post-HSCT BOS, with pulmonary function stabilization or even improvement and steroid sparing. Also, the substantial clinical benefits and efficacy of ruxolitinib on BOS need to be balanced against infection risks.
No relevant conflicts of interest to declare.
Ruxolitinib (RUX, Jakafi, Novartis, Basel, Switzerland)
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal